A percutaneous nephrostomy is an interventional procedure in which a small, flexible rubber tube (catheter) through your skin into your kidney is placed to drain your urine. A thin, hollow tube placed inside the ureter during surgery to ensure drainage of urine from the kidney into the bladder. J shaped curls are present at both ends to hold the tube in place and prevent migration, hence the description “Double J stent”.Minimally invasive therapy in the urinary tract begins with renal access by means of percutaneous nephrostomy. Indications for percutaneous nephrostomy include urinary diversion, treatment of nephrolithiasis and complex urinary tract infections, ureteral intervention, and nephroscopy and ureteroscopy. Bleeding complications can be minimized by entering the kidney in a relatively avascular zone created by the branching of the renal artery. The specific site of renal entry is dictated by the indication for access with consideration of the anatomic constraints. Successful percutaneous nephrostomy requires visualization of the collecting system for the selection of an appropriate entry site.
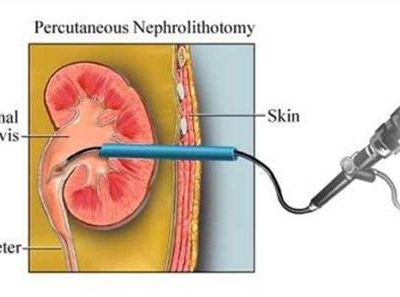
Ureteral stenting and nephrostomy help restore urine flow through blocked ureters and return the kidney to normal function. Ureters are long, narrow tubes that carry urine from the kidneys to the bladder. They can become obstructed – and urine flow blocked – as a result of various conditions. Your doctor may use image guidance to place a thin, flexible tube called a stent into the ureter to restore urine flow. If a stent cannot be placed, he may perform a nephrostomy, during which a tube is placed through the skin into the kidney and connected to either an external drainage bag or the bladder for internal drainage.
Basic Nephrostomy Technique
Patient Preparation
Informed consent should always be obtained and should include a discussion of the reason for the procedure, use of conscious sedation or other forms of anesthesia, and the potential complications attendant to the procedure. The major complications of percutaneous nephrostomy are bleeding and infection. For placement of small-bore nephrostomy tubes (8–10 F), historical screening for a bleeding diathesis is probably sufficient. When large-bore tracks or complex interventions are anticipated or in patients with complex medical conditions, a complete blood cell count, including platelets, and a formal coagulation profile are performed. Coagulation abnormalities should be corrected before any intervention. Urinalysis is performed to screen for possible active urinary infection. Prophylactic, broad-spectrum antibiotic therapy is initiated prior to the procedure for those patients clearly or potentially infected (known urinary tract infection, urinary conduit diversions, obstruction with or without fever, or presumed urosepsis). Results of preprocedural ultrasonography (US) or CT, although not routinely performed, should be reviewed, if available, to avoid potential complications.
Standard Procedure for Initial Entry
The patient is placed on the fluoroscopy table in the prone position. The back and flank are sterilely cleaned and draped. An entry site into the collecting system is selected based on anatomic landmarks determined from prior imaging. After infiltration of the skin and subcutaneous tissues with 1% lidocaine over the selected site respiration is suspended and a 22-gauge needle is passed from a direct posterior approach into the collecting system during vertical posteroanterior fluoroscopy. During the passage, two tactile “pops” can be appreciated. The first occurs as the needle traverses the renal capsule; the second occurs as the needle enters the collecting system. Renal entry is suggested by the movement of the needle tip in concert with the renal outline during the respiratory excursion. Aspiration is performed as the needle is withdrawn, until urine is observed. A urine sample is obtained on entry into the collecting system and sent for culture. Contrast material and air are injected for caliceal definition. Some operators prefer carbon dioxide to air as a contrast material to avoid the unlikely possibility of air embolism.
