Peripheral Artery Disease
Peripheral arterial disease (PAD), also known as a peripheral vascular disease (PVD), is a very common condition. PAD develops most commonly as a result of atherosclerosis, or hardening of the arteries, which occurs when cholesterol and scar tissue build-up, forming a substance called plaque inside the arteries.
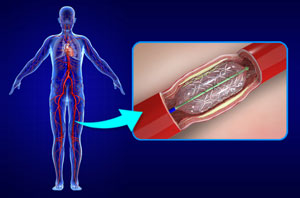
Angioplasty and stenting
Interventional radiologists pioneered angioplasty and stenting, which was first performed to treat peripheral arterial disease. Using imaging for guidance, the interventional radiologist threads a catheter through the femoral artery in the groin, to the blocked artery in the legs. Then the interventional radiologist inflates a balloon to open the blood vessel where it is narrowed or blocked. In some cases, this is then held open with a stent, a tiny metal cylinder. This is a minimally invasive treatment that does not require surgery, just a nick in the skin the size of a pencil tip.
Peripheral arterial angioplasty and stenting is a surgical procedure employed to widen the narrowed arteries in patients with peripheral arterial disease. Peripheral arterial disease is a condition characterized by the narrowing of the peripheral arteries supplying blood to the neck, arms, legs, lower abdomen, and kidneys. Peripheral arterial disease is often caused by the accumulation of fatty deposits (plaques) in the arterial walls, reducing blood flow through them.
Peripheral angioplasty with stenting is a minimally invasive procedure performed to improve blood flow through the blocked peripheral arteries. The procedure is often performed in the cardiac catheterization laboratory with the patient under local anesthesia.
In peripheral angioplasty, a catheter (a small hollow tube) is inserted through a small incision over an artery in the groin. The catheter is guided to the blocked or narrowed section of the artery, under the fluoroscopic (X-ray) guidance. Once in place, a small balloon at the end of the catheter is inflated, pushing the plaque against the arterial walls and widening the vessel, and improving blood flow. The balloon is then deflated and removed from the blood vessel.
Peripheral angioplasty is often combined with the placement of a stent, a small tubular mesh, inside the artery. The stent maintains the patency of the artery and prevents it from future narrowing. Some stents are drug-eluting, meaning they contain a medication that is actively released into the artery, to reduce the risk of re-narrowing.
Angioplasty uses a balloon-tipped catheter to open a blocked blood vessel and improve blood flow. The doctor uses medical imaging to guide the catheter to the blockage. The balloon is inflated to open the vessel and improve blood flow. It may be done with or without a metal mesh tube called a stent. The stent is left inside the blood vessel to help keep it open. Angioplasty is minimally invasive and usually does not require general anesthesia.